MedExpert Science & Research
By MedExpert | Mar 22, 2020 SHARE Q. My 84 year old grandmother has rheumatoid arthritis and COPD. I just found out that her rheumatoid arthritis had been treated with the antimalaria drug Plaquenil, hydroxychloroquine, and the antibiotic, Z Pac, azithromycin, for 10 of the last 12 years. Are there updates on the success of taking hydroxychloroquine in combination with azithromycin? She still has both drugs in her medicine cabinet and does not intend to self-medicate but is encouraged that there may be a treatment for COVID-19.A.
Several days ago Dr. Philippe Gautret published early results from a small study being conducted at The Méditerranée Infection University Hospital Institute in Marseille France. Gautret treated 20 patients infected with SARS-CoV-2 (COVID-19) with hydroxychloroquine and six of those patients were treated with a combination of hydroxychloroqine and azithromycin. The clinical trial is not randomized and the study will continue but early results find that the 20 patients treated with Hydroxychloroquine saw SARS-CoV-2 reduction or disappearance.
A total of 36 patients were studied; 20 were treated with hydroxychloroquine and 16 were control patients. Fifteen patients were male (41.7%), with a mean age of 45.1 years; 16.7 % of the patients were asymptomatic (without any symptoms), 61.1% had upper respiratory tract infection (URTI) and 22.2 % had lower respiratory tract infections (LRTI) and the LRTI patients had cat scan confirmed pneumonia. The hydroxychloroquine-treated patients were older than control patients (51.2 years vs. 37.3 years). Six of the patients treated with hydroxychloroquine also received the antibiotic azithromycin (500mg on day1 followed by 250mg per day, the next four days).
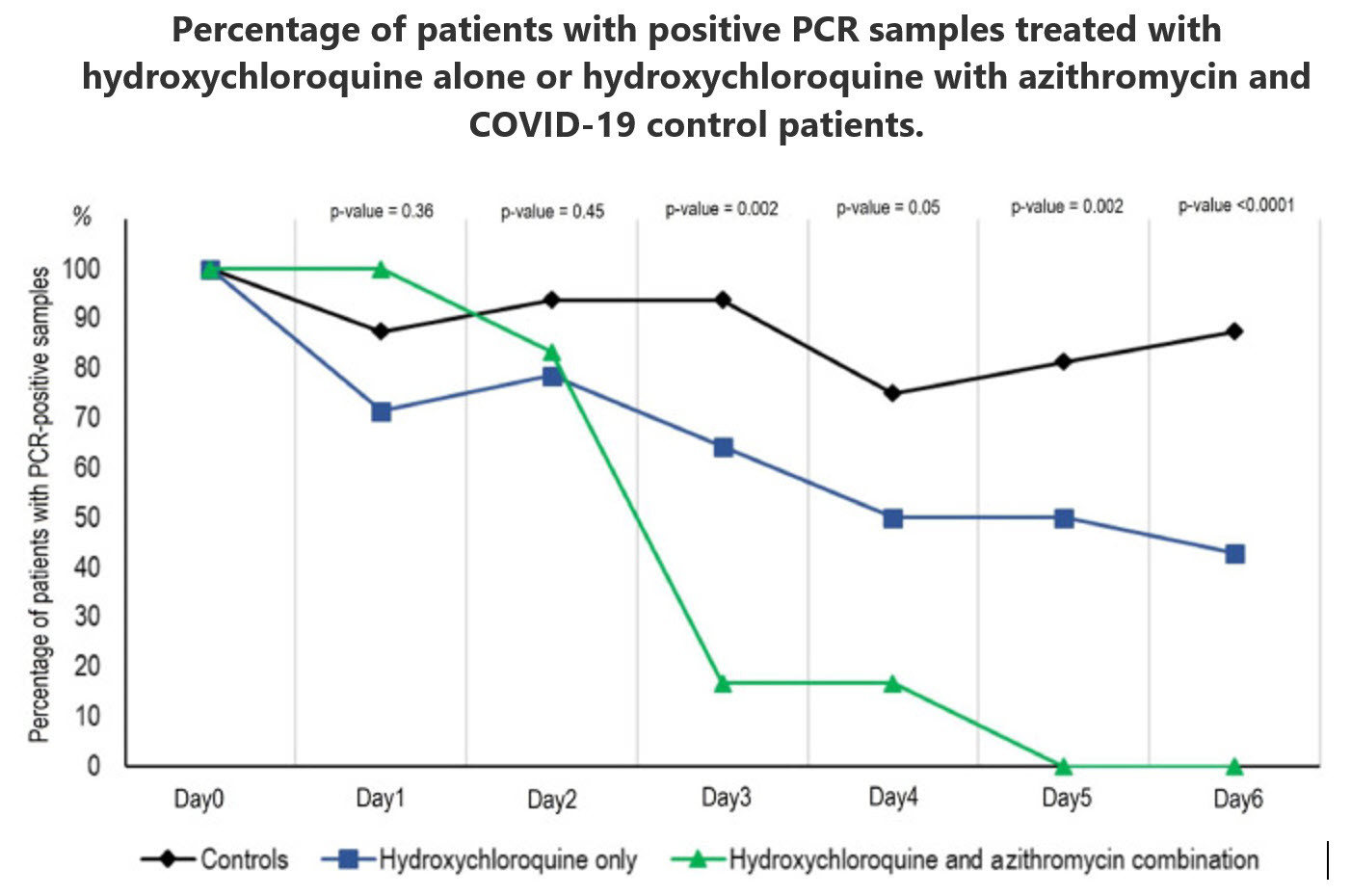
Dr. Philippe Gautret reports in International Journal of Antimicrobial Agents that “At day 6 post-inclusion, 100% of patients treated with hydroxychloroquine and azithromycin combination were virologicaly cured comparing with 57.1% in patients treated with hydroxychloroquine only, and 12.5% in the control group (p<0.001).”
Below is a graph of the results. Researchers often use a technique called polymerase chain reaction or PCR to determine if the gene of a pathogen (in this case, SARS-CoV-2) is present or absent. Originally developed in 1983 by American biochemist Kary Mullis, PCR makes millions of copies of a particular section of DNA to amplify the gene of the pathogen.
The chart identifies the percent of patients who are PCR-positive for SARS-CoV-2 from day 1 to day 6 following the start of either hydroxychloroquine alone which is represented by the blue line or hydroxychloroquine with azithromycin which is represented by the green line. The control group is identified by the black line. The six patients receiving hydroxychloroquine with azithromycin showed a precipitous drop in the presence of SARS-CoV-2 on day 3.
Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial
PhilippeGautretab$Jean-ChristopheLagierac$PhilippeParolaabVan ThuanHoangabdLineMeddebaMorganeMailheaBarbaraDoudieraJohanCourjonefgValérieGiordanengohVera EstevesVieiraaHervé TissotDupontacStéphaneHonoréijPhilippeColsonacEricChabrièreacBernardLa ScolaacJean-MarcRolainacPhilippeBrouquiacDidierRaoultac1. Introduction
In late December 2019, an outbreak of an emerging disease (COVID-19) due to a novel coronavirus (named SARS-CoV-2 latter) started in Wuhan, China and rapidly spread in China and outside [1,2]. The WHO declared the epidemic of COVID-19 as a pandemic on March 12th 2020 [3]. According to a recent Chinese stud, about 80% of patients present with mild disease and the overall case-fatality rate is about 2.3% but reaches 8.0% in patients aged 70 to 79 years and 14.8% in those aged ≥80 years [4]. However, there is probably an important number of asymptomatic carriers in the population, and thus the mortality rate is probably overestimated. France is now facing the COVID-19 wave with more than 4500 cases, as of March 14th 2020 [5]. Thus, there is an urgent need for an effective treatment to treat symptomatic patients but also to decrease the duration of virus carriage in order to limit the transmission in the community. Among candidate drugs to treat COVID-19, repositioning of old drugs for use as antiviral treatment is an interesting strategy because knowledge on safety profile, side effects, posology and drug interactions are well known [6,7]. A recent paper reported an inhibitor effect of remdesivir (a new antiviral drug) and chloroquine (an old antimalarial drug) on the growth of SARS-CoV-2 in vitro, [8] and an early clinical trial conducted in COVID-19 Chinese patients, showed that chloroquine had a significant effect, both in terms of clinical outcome and viral clearance, when comparing to controls groups [9,10]. Chinese experts recommend that patients diagnosed as mild, moderate and severe cases of COVID-19 pneumonia and without contraindications to chloroquine, be treated with 500 mg chloroquine twice a day for ten days [11]. Hydroxychloroquine (an analogue of chloroquine) has been demonstrated to have an anti-SARS-CoV activity in vitro [12]. Hydroxychloroquine clinical safety profile is better than that of chloroquine (during long-term use) and allows higher daily dose [13] and has fewer concerns about drug-drug interactions [14]. Our team has a very comprehensive experience in successfully treating patients with chronic diseases due to intracellular bacteria (Q fever due to Coxiella burnetii and Whipple’s disease due to Tropheryma whipplei) with long-term hydroxychloroquine treatment (600 mg/day for 12 to 18 months) since more than 20 years. [15,16] We therefore started to conduct a clinical trial aiming at assessing the effect of hydroxychloroquine on SARS-CoV-2-infected patients after approval by the French Ministry of Health. In this report we describe our early results, focusing on virological data in patients receiving hydroxychloroquine as compared to a control group.2. Study population and Methods
2.1. Setting
This ongoing study is coordinated by The Méditerranée Infection University Hospital Institute in Marseille. Patients who were proposed a treatment with hydroxychloroquine were recruited and managed in Marseille centre. Controls without hydroxychloroquine treatment were recruited in Marseille, Nice, Avignon and Briançon centers, all located in South France.
2.2. Patients
Hospitalized patients with confirmed COVID-19 were included in this study if they fulfilled two primary criteria: i) age >12 years; ii) PCR documented SARS-CoV-2 carriage in nasopharyngeal sample at admission whatever their clinical status.
Patients were excluded if they had a known allergy to hydroxychloroquine or chloroquine or had another known contraindication to treatment with the study drug, including retinopathy, G6PD deficiency and QT prolongation. Breastfeeding and pregnant patients were excluded based on their declaration and pregnancy test results when required.
2.3. Informed consent
Before being included in the study, patients meeting inclusion criteria had to give their consent to participate to the study. Written informed signed consent was obtained from adult participants (≥ 18 years) or from parents or legal guardians for minors (<18 years). An information document that clearly indicates the risks and the benefits associated with the participation to the study was given to each patient. Patients received information about their clinical status during care regardless of whether they participate in the study or not. Regarding patient identification, a study number was assigned sequentially to included participants, according to the range of patient numbers allocated to each study centre. The study was conducted in accordance with the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) guidelines of good clinical practice, the Helsinki Declaration, and applicable standard operating procedures.
The protocol, appendices and any other relevant documentation were submitted to the French National Agency for Drug Safety (ANSM) (2020-000890-25) and to the French Ethic Committee (CPP Ile de France) (20.02.28.99113) for reviewing and approved on 5th and 6th March, 2020, respectively. This trial is registered with EU Clinical Trials Register, number 2020-000890-25.2.4. Procedure
Patients were seen at baseline for enrolment, initial data collection and treatment at day-0, and again for daily follow-up during 14 days. Each day, patients received a standardized clinical examination and when possible, a nasopharyngeal sample was collected. All clinical data were collected using standardized questionnaires. All patients in Marseille center were proposed oral hydroxychloroquine sulfate 200 mg, three times per day during ten days (in this preliminary phase,we did not enrolled children in the treatment group based in data indicating that children develop mild symptoms of COVID-19 [4]). Patients who refused the treatment or had an exclusion criteria, served as controls in Marseille centre. Patients in other centers did not receive hydroxychloroquine and served as controls. Symptomatic treatment and antibiotics as a measure to prevent bacterial super-infection was provided by investigators based on clinical judgment. Hydroxychloroquine was provided by the National Pharmacy of France on nominative demand.2.5. Clinical classification
Patients were grouped into three categories: asymptomatic, upper respiratory tract infection (URTI) when presenting with rhinitis, pharyngitis, or isolated low-grade fever and myalgia, and lower respiratory tract infections (LRTI) when presenting with symptoms of pneumonia or bronchitis.
2.6. PCR assay
SARS-CoV-2 RNA was assessed by real-time reverse transcription-PCR [17].2.7. Hydroxychloroquine dosage
Native hydroxychloroquine has been dosed from patients’ serum samples by UHPLC-UV using a previously described protocol [18]. The peak of the chromatogram at 1.05 min of retention corresponds to hydroxychloroquine metabolite. The serum concentration of this metabolite is deduced from UV absorption, as for hydroxychloroquine concentration. Considering both concentrations provides an estimation of initial serum hydroxychloroquine concentration.2.8. Culture
For all patients, 500 µL of the liquid collected from the nasopharyngeal swab were passed through 0.22-µm pore sized centrifugal filter (Merck millipore, Darmstadt, Germany), then were inoculated in wells of 96-well culture microplates, of which 4 wells contained Vero E6 cells (ATCC CRL-1586) in Minimum Essential Medium culture medium with 4% fetal calf serum and 1% glutamine. After centrifigation at 4,000 g, microplates were incubated at 37°C. Plates were observed daily for evidence of cytopathogenic effect. Presumptive detection of virus in supernatant was done using SU5000 SEM (Hitachi) then confirmed by specific RT-PCR.
2.9. Outcome
The primary endpoint was virological clearance at day-6 post-inclusion. Secondary outcomes were virological clearance overtime during the study period, clinical follow-up (body temperature, respiratory rate, long of stay at hospital and mortality), and occurrence of side-effects.
2.10. Statistics
Assuming a 50% efficacy of hydroxychloroquine in reducing the viral load at day 7, a 85% power, a type I error rate of 5% and 10% loss to follow-up, we calculated that a total of 48 COVID-19 patients (ie, 24 cases in the hydroxychloroquine group and 24 in the control group) would be required for the analysis (Fleiss with CC). Statistical differences were evaluated by Pearson’s chi-square or Fisher’s exact tests as categorical variables, as appropriate. Means of quantitative data were compared using Student’s t-test. Analyses were performed in Stata version 14.2.
3. Results (detailed results are available in supplementary Table 1)
3.1. Demographics and clinical presentation
We enrolled 36 out of 42 patients meeting the inclusion criteria in this study that had at least six days of follow-up at the time of the present analysis. A total of 26 patients received hydroxychloroquine and 16 were control patients. Six hydroxychloroquine-treated patients were lost in follow-up during the survey because of early cessation of treatment. Reasons are as follows: three patients were transferred to intensive care unit, including one transferred on day2 post-inclusion who was PCR-positive on day1, one transferred on day3 post-inclusion who was PCR-positive on days1-2 and one transferred on day4 post-inclusion who was PCR-positive on day1 and day3; one patient died on day3 post inclusion and was PCR-negative on day2; one patient decided to leave the hospital on day3 post-inclusion and was PCR-negative on days1-2; finally, one patient stopped the treatment on day3 post-inclusion because of nausea and was PCR-positive on days1-2-3. The results presented here are therefore those of 36 patients (20 hydroxychloroquine-treated patients and 16 control patients). None of the control patients was lost in follow-up. Basic demographics and clinical status are presented in Table 1. Overall, 15 patients were male (41.7%), with a mean age of 45.1 years. The proportion of asymptomatic patients was 16.7%, that of patients with URTI symptoms was 61.1% and that of patients with LRTI symptoms was 22.2%). All patients with LRTI symptoms, had confirmed pneumonia by CTScan. Hydroxychloroquine-treated patients were older than control patients (51.2 years vs. 37.3 years). No significant difference was observed between hydroxychloroquine-treated patients and control patients with regard to gender, clinical status and duration of symptoms prior to inclusion (Table 1). Among hydroxychloroquine-treated patients six patients received azithromycin (500mg on day1 followed by 250mg per day, the next four days) to prevent bacterial super-infection under daily electrocardiogram control. Clinical follow-up and occurrence of side-effects will be described in a further paper at the end of the trial.Table 1. Characteristics of the study population.
| Age (years) | Male gender | Clinical status | Time between onset of symptoms and inclusion (days) | |||||||||
| Mean ± SD | t | p-value | n (%) | p-value | Asymptomatic | URTI | LRTI | p-value | Mean ± SD | t | p-value | |
| Hydroxychloroquine treated patients (N=20) | 51.2 ± 18.7 | -1.95 | 0.06 | 9 (45.0) | 0.65 | 2 (10.0) | 12 (60.0) | 6 (30.0) | 0.30 | 4.1 ± 2.6 | -0.15 | 0.88 |
| Control patients (N=16) | 37.3 ± 24.0 | 6 (37.5) | 4 (25.0) | 10 (62.5) | 2 (12.5) | 3.9 ± 2.8 | ||||||
| All patients (36) | 45.1 ± 22.0 | 15 (41.7) | 6 (16.7) | 22 (61.1) | 8 (22.2) | 4.0 ± 2.6 | ||||||
URTI: upper tract respiratory infection, LRTI: lower tract respiratory infection
3.2. Hydroxychloroquine dosage
Mean hydroxychloroquine serum concentration was 0.46 µg/ml±0.2 (N=20).
3.3. Effect of hydroxychloroquine on viral load
The proportion of patients that had negative PCR results in nasopharyngeal samples significantly differed between treated patients and controls at days 3-4-5 and 6 post-inclusion (Table 2). At day6 post-inclusion, 70% of hydroxychloroquine-treated patients were virologicaly cured comparing with 12.5% in the control group (p= 0.001).Table 2. Proportion of patients with virological cure (negative nasopharyngeal PCR) by day, in COVID-19 patients treated with hydroxychloroquine and in COVID-19 control patients.
| Day3 post inclusion | Day4 post inclusion | Day5 post inclusion | Day6 post inclusion | |||||||||
| Number of negative patients/total number of patients | % | p-value | Number of negative patients/total number of patients | % | p-value | Number of negative patients/total number of patients | % | p-value | Number of negative patients/total number of patients | % | p-value | |
| Hydroxychloroquine treated patients (N=20) | 10/20 | 50.0 | 0.005 | 12/20 | 60.0 | 0.04 | 13/20 | 65.0 | 0.006 | 14/20 | 70.0 | 0.001 |
| Control patients (N=16) | 1/16 | 6.3 | 4/16 | 25.0 | 3/16 | 18.8 | 2/16 | 12.5 | ||||
Table 3. Proportion of patients with virological cure (negative nasopharyngeal PCR) by day, in COVID-19 patients treated with hydroxychloroquine only, in COVID-19 patients treated with hydroxychloroquine and azithomycin combination, and in COVID-19 control patients.
| Day3 post inclusion | Day4 post inclusion | Day5 post inclusion | Day6 post inclusion | |||||||||||
| Number of negative patients/total number of patients | % | p-value | Number of negative patients/total number of patients | % | p-value | Number of negative patients/total number of patients | % | p-value | Number of negative patients/total number of patients | % | p-value | |||
| Control patients | 1/16 | 6.3 | 0.002 | 4/16 | 25.0 | 0.05 | 3/16 | 18.8 | 0.002 | 2/16 | 12.5 | <0.001 | ||
| Hydroxychloroquine treatment only | 5/14 | 35.7 | 7/14 | 50.0 | 7/14 | 50.0 | 8/14 | 57.1 | ||||||
| Hydroxychloroquine and azithromycin combined treatment | 5/6 | 83.3 | 5/6 | 83.3 | 6/6 | 100 | 6/6 | 100 | ||||||

Figure 1. Percentage of patients with PCR-positive nasopharyngeal samples from inclusion to day6 post-inclusion in COVID-19 patients treated with hydroxychloroquine and in COVID-19 control patients.

Figure 2. Percentage of patients with PCR-positive nasopharyngeal samples from inclusion to day6 post-inclusion in COVID-19 patients treated with hydroxychloroquine only, in COVID-19 patients treated with hydroxychloroquine and azithomycin combination, and in COVID-19 control patients.
Of note, one patient who was still PCR-positive at day6-post inclusion under hydroxychloroquine treatment only, received azithromycin in addition to hydroxychloroquine at day8-post inclusion and cured her infection at day-9 post infection. In contrast, one of the patients under hydroxychloroquine and azithromycin combination who tested negative at day6 post-inclusion was tested positive at low titer at day8 post-inclusion.
3.4. Cultures
We could isolate SARS-CoV-2 in 19 out of 25 clinical samples from patients.
4. Discussion
For ethical reasons and because our first results are so significant and evident we decide to share our findings with the medical community, given the urgent need for an effective drug against SARS-CoV-2 in the current pandemic context.
We show here that hydroxychloroquine is efficient in clearing viral nasopharyngeal carriage of SARS-CoV-2 in COVID-19 patients in only three to six days, in most patients. A significant difference was observed between hydroxychloroquine-treated patients and controls starting even on day3 post-inclusion. These results are of great importance because a recent paper has shown that the mean duration of viral shedding in patients suffering from COVID-19 in China was 20 days (even 37 days for the longest duration) [19] Very recently, a Chinese team published results of a study demonstrating that chloroquine and hydroxychloroquine inhibit SARS-CoV-2 in vitro with hydroxychloroquine (EC50=0.72%µM) found to be more potent than chloroquine (EC50=5.47%µM) [14]. These in vitro results corroborate our clinical results. The target values indicated in this paper [14] were reached in our experiments. The safer dose-dependent toxicity profile of hydroxychloroquine in humans, compared to that of chloroquine [13] allows using clinical doses of hydroxychloroquine that will be over its EC50 observed in vitro [14]. Our preliminary results also suggest a synergistic effect of the combination of hydroxychloroquine and azithromycin. Azithromycin has been shown to be active in vitro against Zika and Ebola viruses [20], [21], [22] and to prevent severe respiratory tract infections when administrated to patients suffering viral infection [23]. This finding should be further explored to know whether a combination is more effective especially in severe cases. Speculated potential risk of severe QT prolongation induced by the association of the two drugs has not been established yet but should be considered. As for each treatment, the cost benefits of the risk should be evaluated individually. Further studies on this combination are needed, since such combination may both act as an antiviral therapy against SARS-CoV-2 and prevent bacterial super-infections.The cause of failure for hydroxychloroquine treatment should be investigated by testing the isolated SARS-CoV-2 strains of the non-respondents and analyzing their genome, and by analyzing the host factors that may be associated with the metabolism of hydroxychloroquine. The existence of hydroxychloroquine failure in two patients (mother and son) is more suggestive of the last mechanism of resistance.
Such results are promising and open the possibility of an international strategy to decision-makers to fight this emerging viral infection in real-time even if other strategies and research including vaccine development could be also effective, but only in the future. We therefore recommend that COVID-19 patients be treated with hydroxychloroquine and azithromycin to cure their infection and to limit the transmission of the virus to other people in order to curb the spread of COVID-19 in the world. Further works are also warranted to determine if these compounds could be useful as chemoprophylaxis to prevent the transmission of the virus, especially for healthcare workers. Our study has some limitations including a small sample size, limited long-term outcome follow-up, and dropout of six patients from the study, however in the current context, we believe that our results should be shared with the scientific community.
Declaration of Competing Interest
N/A
Acknowledgements
We thank Céline Boschi, Stéphanie Branger, Véronique Filosa, Géraldine Gonfier, Nadège Palmero, Magali Richez and all the clinical, technical and paramedical staffs of the hospitalization units and laboratories for their support in this difficult context.
Funding
This work was supported by the French Government under the « Investissements d’avenir » (Investments for the Future) program managed by the Agence Nationale de la Recherche (ANR, fr: National Agency for Research), (reference: Méditerranée Infection 10-IAHU-03)
Ethical Approval
French Ethic Committee (CPP Ile de France) (20.02.28.99113)
Appendix. Supplementary materials
Download : Download Word document (21KB)References
[1]CC Lai, TP Shih, WC Ko, HJ Tang, PR HsuehSevere acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges
Int J Antimicrob Agents (2020 Feb 17), Article 105924, 10.1016/j.ijantimicag.2020.105924
[Epub ahead of print]
ArticleDownload PDFGoogle Scholar
LS Wang, YR Wang, DW Ye, QQ LiuA review of the 2019 Novel Coronavirus (COVID-19) based on current evidence”
Int J Antimicrob Agents (2020)
[Epub ahead of print]
WHO Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020. [https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020]
Z Wu, JM. McGooganCharacteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention
JAMA (2020 Feb 24), 10.1001/jama.2020.2648
[Epub ahead of print]
Santé Publique France. Infection au nouveau Coronavirus (SARS-CoV-2), COVID-19, France et Monde [https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/articles/infection-au-nouveau-coronavirus-sars-cov-2-covid-19-france-et-monde]
P Colson, JM Rolain, D RaoultChloroquine for the 2019 novel coronavirus SARS-CoV-2
Int J Antimicrob Agents (2020 Feb 15), Article 105923, 10.1016/j.ijantimicag.2020.105923
[Epub ahead of print]
ArticleDownload PDFGoogle Scholar
P Colson, JM Rolain, JC Lagier, P Brouqui, D RaoultChloroquine and hydroxychloroquine as available weapons to fight COVID-19
Int J Antimicrob Agents (2020)
[Epub ahead of print]
M Wang, R Cao, L Zhang, X Yang, J Liu, M Xu, et al.Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro
Cell Res (2020), pp. 10-0282
J Gao, Z Tian, X YangBreakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies
Biosci Trends (2020 Feb 19), 10.5582/bst.2020.01047
[Epub ahead of print]
Chinese Clinical Trial Registry. http://www.chictr.org.cn/ searchproj.aspx?title=%E6%B0%AF%E5%96%B9&offi cialname=&subjectid=&secondaryid=&applier=&study leader=ðicalcommitteesanction=&sponsor=&studya ilment=&studyailmentcode=&studytype=0&studystage= 0&studydesign=0&minstudyexecutetime=&maxstudyexe cutetime=&recruitmentstatus=0&gender=0&agreetosign =&secsponsor=®no=®status=0&country=&prov ince=&city=&institution=&institutionlevel=&measure= &intercode=&sourceofspends=&createyear=0&isupload rf=&whetherpublic=&btngo=btn&verifycode=&page=1.
Multicenter collaboration group of Department of Science and Technology of Guangdong Province and Health Commission of Guangdong Province for chloroquine in the treatment of novel coronavirus pneumonia. Expert consensus on chloroquine phosphate for the treatment of novel coronavirus pneumonia]
Zhonghua Jie He He Hu Xi Za Zhi, 43 (3) (2020 Mar 12), pp. 185-188, 10.3760/cma.j.issn.1001-0939.2020.03.009
C Biot, W Daher, N Chavain, T Fandeur, J Khalife, D Dive, et al.Design and synthesis of hydroxyferroquine derivatives with antimalarial and antiviral activities
J Med Chem, 49 (2006), pp. 2845-2849
CrossRefView Record in ScopusGoogle Scholar
MF Marmor, U Kellner, TY Lai, RB MellesMieler WF; American Academy of Ophthalmology. Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision)
Ophthalmology (6) (2016 Jun;123), pp. 1386-1394, 10.1016/j.ophtha.2016.01.058
Epub 2016 Mar 16
ArticleDownload PDFView Record in ScopusGoogle Scholar
X Yao, F Ye, M Zhang, C Cui, B Huang, P Niu, et al.In Vitro Antiviral Activity and Projection of Optimized Dosing Design of Hydroxychloroquine for the Treatment of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)
Clin Infect Dis (2020 Mar 9), 10.1093/cid/ciaa237
pii: ciaa237[Epub ahead of print]
D Raoult, P Houpikian, H Tissot Dupont, JM Riss, J Arditi-Djiane, P BrouquiTreatment of Q fever endocarditis: comparison of 2 regimens containing doxycycline and ofloxacin or hydroxychloroquine
Arch Intern Med, 159 (2) (1999 Jan 25), pp. 167-173
View Record in ScopusGoogle Scholar
JC Lagier, D RaoultWhipple’s disease and Tropheryma whipplei infections: when to suspect them and how to diagnose and treat them
Curr Opin Infect Dis, 31 (6) (2018 Dec), pp. 463-470, 10.1097/QCO.0000000000000489
[x] Expert consensus on chloroquine phosphate for the treatment of novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi. 2020 Mar 12;43(3):185-188. doi: 10.3760/cma.j.issn.1001-0939.2020.03.009
CrossRefView Record in ScopusGoogle Scholar
S Amrane, H Tissot-Dupont, B Doudier, C Eldin, M Hocquart, M Mailhe, et al.Rapid viral diagnosis and ambulatory management of suspected COVID-19 cases presenting at the infectious diseases referral hospital in Marseille, France, – January 31st to March 1st, 2020: A respiratory virus snapshot
Travel Med Infect Dis. (2020)
[Epub ahead of print]
N Armstrong, M Richez, D Raoult, E ChabriereSimultaneous UHPLC-UV analysis of hydroxychloroquine, minocycline and doxycycline from serum samples for the therapeutic drug monitoring of Q fever and Whipple’s disease
J. Chromatogr. B Analyt. Technol. Biomed. Life Sci., 1060 (2017), pp. 166-172
ArticleDownload PDFView Record in ScopusGoogle Scholar
F Zhou, T Yu, R Du, G Fan, Y Liu, Z Liu, et al.Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
Lancet (2020 Mar 11), 10.1016/S0140-6736(20)30566-3
pii: S0140-6736(20)30566-3[Epub ahead of print]
H Retallack, E Di Lullo, C Arias, KA Knopp, MT Laurie, C Sandoval-Espinosa, et al.Zika virus cell tropism in the developing human brain and inhibition by azithromycin
Proc Natl Acad Sci U S A, 113 (50) (2016 Dec 13), pp. 14408-14413
Epub 2016 Nov 29
CrossRefView Record in ScopusGoogle Scholar
PB Madrid, RG Panchal, TK Warren, AC Shurtleff, AN Endsley, CE Green, A Kolokoltsov, et al.Evaluation of Ebola Virus Inhibitors for Drug Repurposing
ACS Infect Dis, 1 (7) (2015 Jul 10), pp. 317-326, 10.1021/acsinfecdis.5b00030
Epub 2015 May 11
CrossRefView Record in ScopusGoogle Scholar
E Bosseboeuf, M Aubry, T Nhan, JJ de Pina, JM Rolain, D Raoult, et al.Azithromycin inhibits the replication of Zika virus
J Antivirals Antiretrovirals, 10 (1) (2018), pp. 6-11, 10.4172/1948-5964.1000173
View Record in ScopusGoogle Scholar
LB Bacharier, TW Guilbert, DT Mauger, S Boehmer, A Beigelman, AM Fitzpatrick, et al.Early administration of azithromycin and prevention of severe lower respiratory tract illnesses in preschool children with a history of such illnesses: A randomized clinical trial
JAMA, 314 (19) (2015 Nov 17), pp. 2034-2044, 10.1001/jama.2015.13896
10025